Sperm Count: Procedure, Preparation, and Interpretation of Results
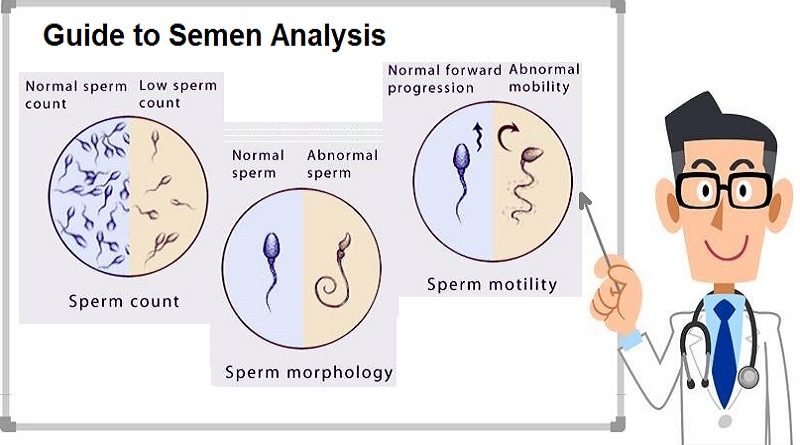
Semen analysis, often referred to as a sperm count test, is a diagnostic procedure used to evaluate male fertility. It can also help to identify underlying reproductive issues. This test provides insights into sperm health by measuring several parameters, like the number, shape, movement, and quality of sperm. Whether you are planning to start a family or assessing reproductive health, understanding semen analysis is important.
This article will cover the following topics:
- Purpose of Semen Analysis
- The procedure of a Semen Analysis
- How to Prepare for a Sperm Test
- Interpretation of Results
- Diseases Diagnosed Through Semen Analysis
- How to Check Your Sperm Count at Home
Purpose of Semen Analysis Procedure
This test is primarily conducted to evaluate male fertility and investigate potential issues when a couple is facing difficulties conceiving. In cases of infertility, male factors account for about 40-50%, making semen analysis an essential first step in determining the cause. Beyond fertility concerns, a semen analysis can also be used to check for the effectiveness of vasectomy procedures or to diagnose certain underlying medical conditions that can affect reproductive health. The main objectives of semen analysis include:
1- Sperm count
It refers to the number of sperm in a semen volume, typically measured in millions per milliliter (mL). It is an important factor in male fertility. Here’s a breakdown of sperm count categories:
– Normal sperm count: Typically ranges from 15 million to over 200 million sperm per milliliter of semen, (15million:200million/mL).
– A low sperm count, known as oligospermia, occurs when the count is fewer than 15 million sperm per milliliter.
– High sperm count: Though not commonly used as a clinical term, a count significantly higher than average usually doesn’t imply any issues.
2- Sperm motility
This refers to the ability of sperm to move efficiently. Proper movement is essential because sperm must swim through the female reproductive system to reach and fertilize an egg. Sperm motility is classified into different types:
– Progressive motility: Sperm move in a straight line. This type of movement is ideal for reaching the egg.
– Non-progressive motility (sluggish): Sperm move but in small, non-linear circles (around itself).
– Immotility (dead): Sperm does not move at all.
The normal values for sperm motility are typically categorized as follows, based on the percentage of moving sperm and the type of movement:
- Total motility (includes both progressive and non-progressive movements):
- At least 40% of sperm should be motile (moving).
- Progressive motility (sperm that moves in a straight line or large circles, which is necessary for fertilization):
- At least 32% should show progressive motility.
These values are based on the World Health Organization (WHO) guidelines for semen analysis. Low motility (below these thresholds) is referred to as asthenozoospermia and can reduce the chances of fertilization, even if the sperm count is normal.
3- Sperm morphology
It refers to the size and shape of sperm, and it plays a crucial role in fertility. Healthy sperm typically have an oval head, an acrosome (enzyme cap) to penetrate the egg, and a long tail for motility. Abnormal sperm have defects in the head, midpiece, or tail, and this can affect their ability to fertilize an egg.
- Normal sperm morphology: Typically, at least 5% to 10% of sperm should have a normal shape. A higher percentage of abnormally shaped sperm can reduce the chances of fertilization. Defects include:
– Head abnormalities: Enlarged, tapered, or double heads
– Tail abnormalities: Coiled, short tails or multiple tails.
– Midpiece abnormalities: Thick or irregularly shaped midpieces
Low sperm morphology, known as teratozoospermia, can decrease fertility, though it doesn’t always mean infertility. Other factors, like sperm count and motility, are also important for overall fertility potential.
4- Semen volume
The normal values for semen volume, as defined by the World Health Organization (WHO), are 1.5 to 7.5 milliliters (mL) per ejaculation.
Seminal volume is important because it contains sperm and other fluids that help transport sperm through the female reproductive system. Low semen volume, known as (hypospermia), can be a sign of issues: blocked ducts or hormonal imbalances, and it can affect fertility. High semen volume can indicate other health conditions but is less commonly a cause for concern unless paired with other abnormalities.
If semen volume is below 1.5 mL, it can reduce the overall number of sperm in the ejaculate, potentially affecting fertility.
5- pH levels
Semen pH levels measure the acidity or alkalinity of the fluid and are an important factor in sperm health. The normal range of semen pH is slightly alkaline: 7.2 to 8.0. A pH level outside this range can cause potential issues:
– High pH (alkaline semen): Above 8.0, can suggest an infection in the reproductive system, as infections often make semen more alkaline.
– Low pH (acidic semen): Below 7.2, can indicate blockages in the seminal vesicles or issues in the prostate, which can negatively affect sperm functions.
2. Procedure of a Semen Analysis
Collecting and analyzing a semen sample is straightforward but must be done carefully to give correct results. Here is a step-by-step outline of the typical procedure:
- Sample Collection:
The patient is usually instructed to collect a semen sample through masturbation into a sterile container. The sample must be collected in a private, clean environment: a laboratory collection room or at home with proper storage conditions. - Sample Handling:
If the sample is collected at home, it needs to be delivered to the lab within one hour, kept at body temperature (around 37°C) to ensure the integrity of the sample. Laboratories have to provide patients with special containers that maintain the required temperature. - Laboratory Analysis:
Once the sample reaches the lab, it is analyzed under a microscope. Parameters like sperm count, motility, morphology, and volume are measured.
It is often recommended that multiple samples be provided over a few weeks to obtain the most correct representation of sperm quality, as factors like illness or stress can temporarily affect sperm count and quality.
3. How Do I Prepare for a Sperm Test?
Preparing for a sperm test requires you to follow certain guidelines to be sure that the results are correct. Here are some preparation tips:
- Abstinence: Refrain from ejaculation or sex for at least 2-5 days before the test. Ejaculating too soon can result in a lower sperm count, while waiting too long can reduce sperm motility.
- Avoid Alcohol Caffeine and smoking, as these can negatively impact sperm quality.
- Medications: Consult your doctor about any medications you are taking, as some drugs can affect sperm production or motility.
- Avoid Heat: Stay away from hot tubs, saunas, or any source of excessive heat to the testicles for a few days before the test, as this can impair sperm production.
- Stay Healthy: be sure you are not suffering from a fever, cold, or any temporary illness, as these conditions can reduce sperm count.
4. Results Interpretation
Once the semen analysis is completed, you will get a detailed report that can be challenging to interpret without guidance. Here’s what the results typically cover:
- Sperm Count: The normal range is 15 million sperm per milliliter or more. Anything below this indicates a low sperm count (oligospermia).
- Sperm Motility: This measures the percentage of sperm that move efficiently. A normal motility rate is 40% or higher.
- Sperm Morphology: Normal sperm morphology should be at 4% or higher sperm having a standard shape.
- Volume: Normal semen volume is between 1.5 and 5 milliliters. Low semen volume can indicate an issue with seminal vesicles or blockages.
- pH Levels: The normal pH range for semen is 7.2 to 8.0. An abnormal pH level can point to infections or other health conditions.
5. What Diseases Can Be Diagnosed by Semen Analysis?
It can reveal more than just fertility status. Certain health conditions and diseases can be diagnosed through abnormal semen analysis results, including:
- Hormonal Imbalances: Low sperm count or poor sperm motility may indicate hormonal imbalances, like low testosterone.
- Infections: A high number of white blood cells in the semen may point to an infection in the reproductive tract, like prostatitis or an STI.
- Genetic Disorders: Poor sperm morphology or low count can be related to genetic disorders like Klinefelter syndrome.
- Varicocele: This is an enlargement of veins in the scrotum that can reduce sperm production and motility.
- Obstruction in Reproductive Tract: Blockages in the vas deferens or other parts of the reproductive system can result in low or no sperm in the semen.
6. How Can I Check My Sperm Analysis Procedure at Home?
For those who prefer the convenience of testing their sperm count at home, several over-the-counter sperm test kits are available. These kits provide a general assessment of sperm count but are not as comprehensive as lab-based semen analyses. Here’s how you can check your sperm count at home:
- Home Test Kits: These kits often work by measuring the concentration of sperm in the semen. The process involves collecting a sample, placing it on a testing device, and waiting for results. Typically, the test will indicate whether your sperm count is above or below a certain threshold (e.g., 15 million sperm per milliliter).
- Limitations: While home test kits offer convenience, they do not provide information on sperm motility or morphology. If your home test results are abnormal, it’s advisable to follow up with a healthcare provider for a full semen analysis.
Conclusion
Semen analysis Procedure is important in diagnosing male fertility issues and detecting underlying health conditions. Whether conducted for family planning or general health concerns, it provides a comprehensive view of sperm health. While at-home test kits can offer a quick check on sperm count, laboratory-based semen analysis remains the gold standard for evaluating all aspects of sperm quality.