The Essential Role of Vitamin D: More Than Just a Vitamin
The role of vitamin D is unique because, strictly speaking, it is not a vitamin; it’s a prohormone. True vitamins must come solely from food. But our bodies can manufacture Vitamin D when the skin is exposed to sunlight. The form we get from both the sun and food is known as Vitamin D3(Cholecalciferol).
The critical importance for the role of Vitamin D extends far beyond its well-known role in bone health. It is essential for the health of the entire body, supporting immune function, muscle movement, and cellular growth.
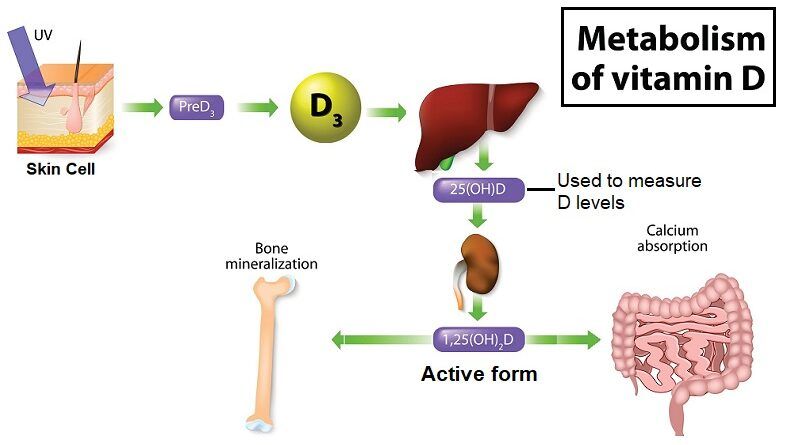
The Metabolism and Activation of Vitamin D
Vitamin D3 has no biological effect until it is chemically transformed within the body. This activation process occurs in two primary steps:
- First Step (Liver): In the liver, Vitamin D3 is converted into the circulating storage form, 25-hydroxyvitamin D (also correctly known as 25-OH D or Calcidiol).
- Second Step (Kidneys): In the kidneys, 25 OH D is converted into the biologically active hormone, 1,25-dihydroxyvitamin D (also known Calcitriol). This is the active form that regulates body functions.
Control of Production
The liver’s production of 25-OH D is only slightly regulated, meaning its the blood level is the best indicator of the total Vitamin D available from sun exposure and diet.
In contrast, the conversion step in the kidneys is precisely controlled by an enzyme called $1\alpha\text{-hydroxylase}$. This enzyme’s activity is tightly regulated by Parathyroid Hormone (PTH), secreted by the parathyroid glands.
An Interesting Fact
Humans, along with many other mammals (horses, pigs, cattle), have sufficient raw material in their skin (7-dehydrocholesterol) to make $\text{D}_3$ from the sun. However, species like dogs and cats have very little of this precursor and must rely on food for nearly all their Vitamin D intake.
Key Benefits and Role of Vitamin D
1. Essential Body Functions
The most thoroughly understood function of Vitamin D is the regulation of calcium and phosphorus metabolism. Vitamin D is crucial for absorbing calcium from the digestive system (intestine) and maintaining optimal mineral levels for:
- Bone Strength: Achieving adequate mineralization of the skeleton.
- Preventing Disease: Severe deficiency leads to bone diseases: Rickets in children (causing bowed legs and bone deformation) and Osteomalacia (softening of the bones) in adults.
2. Protection and Health Support
Beyond bone health, Vitamin D is needed for:
- Immune System Support
- Muscular and Nervous System Function
- Cellular Health
While research has linked low Vitamin D levels to an increased risk of chronic conditions (including certain cancers, heart disease, depression, and diabetes), solid scientific evidence confirming that Vitamin D deficiency directly causes these diseases is still developing. Currently, the most conclusive benefit remains its proven role in building and maintaining strong bones via calcium and phosphorus regulation.
Measuring and Understanding Vitamin D Status
The Best Measure: $25\text{-hydroxyvitamin D}$ ($25(\text{OH})\text{D}$)
Although $1,25\text{-dihydroxyvitamin D}$ is the active hormone, it is not the recommended test for Vitamin D status. Instead, laboratories measure the storage form, $25\text{-hydroxyvitamin D}$ ($25(\text{OH})\text{D}$), for several critical reasons:
- Longevity: $25(\text{OH})\text{D}$ has a much longer half-life (2-3 weeks) compared to the active form (4-6 hours).
- Quantity: Its blood levels are 1,000 times higher, making measurement easier and more reliable.
- Reliability: In cases of deficiency, the body increases PTH secretion. This high PTH actively forces the kidneys to maximize production of $1,25(\text{OH})_2\text{D}$. This compensatory mechanism can keep the active hormone level normal or even elevated despite low Vitamin D stores, making it useless as a measure of overall status.
Normal Vitamin D Levels
Most experts agree on the following general ranges for $25(\text{OH})\text{D}$:
- Deficient: Less than $10 \text{ ng/ml}$ (severe deficiency).
- Ideal: Between $30$ and $80 \text{ ng/ml}$.
- Excessive/Toxicity Risk: $80 \text{ ng/ml}$ or more.
Causes and Symptoms of Deficiency
Why is Deficiency Common?
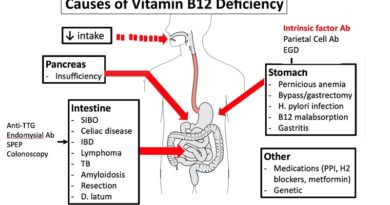
Vitamin D deficiency is widespread due to several factors:
- Lack of Sun Exposure: Living at high latitudes, working/staying indoors, and using protective clothing.
- Skin Pigmentation: Darker skin pigment (melanin) reduces the amount of UV radiation absorbed, requiring longer sun exposure to make the same amount of Vitamin D as fair skin.
- Health Conditions: Chronic kidney disease or malabsorption syndromes.
Symptoms of Deficiency
Vitamin D deficiency causes demineralization of bone (osteoporosis/osteomalacia).
- In Children: The first sign may be hypocalcemia (low calcium levels), followed by signs of Rickets (e.g., bowed legs).
- In Adults: Symptoms can be vague, such as lethargy, low mood, or muscle aches, but severe deficiency leads to Osteomalacia and an unsteady gait.
How to Get Enough Vitamin D
The body’s requirement for Vitamin D can be met through sun exposure and dietary sources.
1. Sunlight Exposure
The body can synthesize a good amount of Vitamin D from 15 minutes of sun exposure daily, or half an hour at least twice a week. However, direct exposure to UV rays in large amounts carries the risk of skin damage and cancer.
2. Food and Supplements
For those who cannot get enough sun exposure safely, food and supplements are essential:
- Top Food Sources: Fatty fish like Salmon, Mackerel, and Tuna.
- Other Sources: Cod liver oil (also rich in Omega-3s), sardines, egg yolks, fortified dairy products (milk, yogurt), and beef/calf liver.
Consult with a healthcare provider to determine the right course of action, which often includes a combination of safe sun exposure, fortified foods, and/or nutritional supplements.
Sources and References:
https://pubmed.ncbi.nlm.nih.gov/16563471/
https://www.mayoclinicproceedings.org/article/S0025-6196(12)64791-0/fulltext
https://www.webmd.com/osteoporosis/features/the-truth-about-vitamin-d-why-you-need-vitamin-d
https://www.health.harvard.edu/blog/vitamin-d-whats-right-level-2016121910893
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2912737/
We are in December:
- Read about Managing Stress During the Holiday for Better Heart Health
- 💬 Chat with Us:
- You can easily reach Helal Medical via WhatsApp (+63 966 974 1609), Facebook Messenger, or by clicking the chat icon at the lower right corner of our website HelalMedical.com.