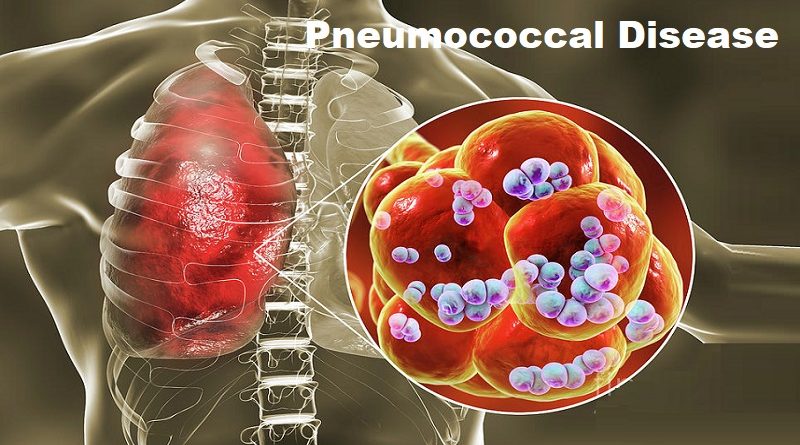
Pneumococcal Disease: Unveiling the Silent Threat
Pneumococcal disease, a potentially serious respiratory infection caused by the bacterium Streptococcus pneumoniae, is a global health concern that often goes unnoticed. Despite being preventable, it continues to claim countless lives, particularly among vulnerable populations. In this article, we will explore the nature of pneumococcal disease, its causes, symptoms, risk factors, and the importance of prevention strategies.
Understanding Pneumococcal Disease
Pneumococcal disease refers to a range of infections caused by the bacterium Streptococcus pneumoniae. It can affect various parts of the body, including the lungs (pneumonia), blood (bacteremia), and the covering of the brain (meningitis). Pneumococcal bacteria can be found in the upper respiratory tract of many individuals, often without causing any harm. However, under certain circumstances, these bacteria can invade other parts of the body, leading to infection and potentially life-threatening complications.
The Causes and Transmission
Pneumococcal bacteria are highly contagious and can spread from person to person through respiratory droplets. Common modes of transmission include coughing, sneezing, and close contact with an infected individual. Additionally, these bacteria can also be present in the nasopharynx of healthy individuals, serving as a reservoir for further spread. Certain risk factors, such as a weakened immune system, chronic illness, and crowded living conditions, increase the likelihood of acquiring pneumococcal disease.
Symptoms and Complications
The symptoms of pneumococcal disease can vary depending on the site of infection. In cases of pneumonia, individuals may experience high fever, cough with phlegm, chest pain, and difficulty breathing. Bacteremia, which occurs when pneumococcal bacteria enter the bloodstream, can cause symptoms such as fever, chills, rapid breathing, and low blood pressure. Meningitis, the infection of the brain’s covering, presents with severe headache, neck stiffness, sensitivity to light, and altered mental status.
If left untreated, pneumococcal disease can lead to severe complications. These include lung abscesses, septic shock, organ failure, and even death. Certain groups, such as young children, older adults, individuals with weakened immune systems, and those with chronic health conditions, are at higher risk of developing complications.
Diagnosis of pneumonia
For diagnosis of Pneumonia, we usually combine medical history, physical examination, and diagnostic tests. The common steps in diagnosing pneumonia include:
- Medical history:
This includes your symptoms, any recent illnesses, travel history, or exposure to respiratory infections. - Physical examination:
Done by the doctor to find signs such as abnormal breathing sounds, (crackles or decreased breath sounds). Other signs include fever, rapid breathing, or low oxygen levels in your blood. - Chest X-ray:
Chest X-rays can detect abnormalities in the lungs, such as inflammation, consolidation (dense areas caused by fluid or infection), or infiltrates (patches of infection). - Blood tests:
To help assess the severity of infection and identify the causative organism. These tests include complete blood count (CBC) which measures the number of white blood cells, and C-reactive protein (CRP) which can indicate the presence of infection. - Sputum examination and culture:
Testing a sample is tested to identify the specific causative agent, (bacteria, virus, or fungus). - Pulse oximetry:
Many are familiar with this method, as it was commonly used during the Covid-19 pandemic. This non-invasive test measures the oxygen saturation in your blood by placing a sensor on your finger or earlobe. Low oxygen levels may suggest a pneumonia-related respiratory compromise. - Additional tests:
Such as computed tomography (CT) scans or bronchoscopy (visual examination of the airways), may be necessary to further evaluate the lungs or obtain a better sample for testing.
Treatment
The treatment is usually by a combination of medications, rest, and supportive care, including the following:
- Antibiotics:
for pneumonia caused by bacteria, antibiotics can eliminate the infection. The choice of antibiotic depends on the specific bacteria involved and the severity of the infection. Sputum culture and sensitivity test can show the most sensitive (effective) antibacterials - Antiviral drugs:
Viral pneumonia is often managed with supportive care to relieve symptoms. Antiviral medications can be used. but they are not available for all types of viruses. - Fever and pain relief:
Over-the-counter medications like acetaminophen or ibuprofen help reduce symptoms such as fever, pain, and discomfort. - Cough medications:
These are medications used to reduce or suppress coughing. They work by suppressing the cough reflex in the brain. They are helpful in relieving cough symptoms, particularly when the cough is persistent and causing discomfort or interfering with sleep. - Plenty of rest and fluids:
Getting adequate rest and hydrated is crucial for the body to fight off the infection. Drink plenty of fluids like water, and herbal tea. - Oxygen therapy:
In severe cases, supplemental oxygen may be necessary to ensure the body receives enough oxygen. Oxygen therapy can be administered using a face mask or nasal prongs. - Hospitalization:
If the condition is severe, particularly in older adults, infants, or individuals with underlying health conditions, hospitalization may be required, for intravenous antibiotics and close monitoring.
Prevention Strategies
Fortunately, there are effective prevention strategies to combat pneumococcal disease:
1- Vaccination:
Vaccination is the most crucial measure to prevent pneumococcal disease. The pneumococcal conjugate vaccine (PCV) and the pneumococcal polysaccharide vaccine (PPSV) are available to protect against different strains of Streptococcus pneumoniae. PCV is recommended for infants and young children, while PPSV is typically administered to older children and adults at increased risk.
2- Hygiene Practices:
Practicing good hygiene can help reduce the risk of pneumococcal disease transmission. Regular handwashing with soap and water, covering the mouth and nose when coughing or sneezing, and avoiding close contact with infected individuals are essential preventive measures.
3- Healthy Lifestyle:
Maintaining a healthy lifestyle can enhance the body’s immune response and reduce the risk of infection. Eating a balanced diet, getting regular exercise, managing stress levels, and avoiding smoking are all factors that contribute to overall well-being and immune function.
Summary:
Pneumococcal disease is a potentially serious infection caused by Streptococcus pneumoniae. This article explores its causes, symptoms, and complications, emphasizing the significance of prevention strategies such as vaccination. Discover how to protect yourself and others from this silent threat.
If you suspect that you may have contracted pneumococcal infections, Helal medical can offer quick, convenient testing options.
Visit our Facebook page.